Running a dermatology practice today requires more than excellent patient care. With rising drug costs, shifting payer rules, constant coding updates, and increased carrier denials, the financial health of your practice depends on whether your team is capturing every legitimate dollar. Among the most important, but often misunderstood, are the areas of billing J codes and Q codes. These codes are the key to getting reimbursed for expensive drugs, biologics, and tissue substitutes. If your practice doesn’t understand the often-complex guidelines, you could be leaving thousands of dollars uncollected.
What Are J Codes?
J codes are permanent HCPCS Level II codes used to report drugs and biologics. They allow payers to identify the exact medication administered, the dosage, and the way it was supplied. In dermatology, J codes show up most often in treatments for psoriasis, atopic dermatitis, acne, and certain skin cancers.
By understanding the reimbursement guidelines, providers can expect payment that offsets the cost of purchasing and administering these drugs. Missing or misusing J codes often results in significant revenue loss since these are rarely inexpensive medications.
Common Dermatology J Codes
Code | Description | Dermatology Use Case |
J7318 | Mitomycin, ophthalmic, 0.2 mg | Sometimes used off-label in dermatologic surgery (scar prevention, keloid treatment). |
J7319 | Injection, bimatoprost, 0.1 mg | Cosmetic dermatology (eyelash growth), though less commonly billed in medical dermatology. |
J7320 | Hyaluronan or derivative, for intra-articular injection, per dose | Occasionally used for scar tissue and joint-related procedures in derm surgery clinics. |
J7321–J7329 series | Hyaluronic acid and derivatives | Cosmetic and reconstructive dermatology for tissue support and scar revision (varies by product). |
J3357 | Ustekinumab, 1 mg | Biologic therapy for psoriasis. |
J3358 | Ustekinumab, 1 mg (different formulation/packaging) | Biologic therapy for psoriasis. |
J3380 | Vedolizumab, 300 mg | Rare in derm, but used in patients with overlapping inflammatory conditions. |
J3490 | Unclassified drugs | Often used temporarily for dermatology injectables before specific J/Q assignment. |
J3590 | Unclassified biologics | Common placeholder for new dermatology biologics before permanent assignment. |
J7307 | Etonogestrel contraceptive implant | May be placed in dermatology settings that provide hormone or acne-related care. |
J7312 | Mitomycin injection, 0.1 mg | Sometimes applied in dermatology for adjunctive surgical use. |
J7314 | Collagen, per mg | Injectable collagen for cosmetic and reconstructive purposes. |
J7316 | Hyaluronic acid injection, per dose | Dermal filler use (cosmetic and reconstructive dermatology). |
J9315 | Rituximab, 100 mg | Rare, but sometimes used in autoimmune-related dermatologic conditions. |
J9320 | Alemtuzumab, 10 mg | Very rare in derm, but included as an immune therapy example. |
J1745 | Infliximab, 10 mg | Biologic therapy for severe psoriasis and off-label dermatologic autoimmune conditions. |
J0178 | Aflibercept injection, 1 mg | Occasionally relevant for dermatology oncology overlap cases. |
J1200 | Diphenhydramine injection, per 50 mg | Used in dermatology practices to manage allergic reactions during infusions. |
What Are Q Codes?
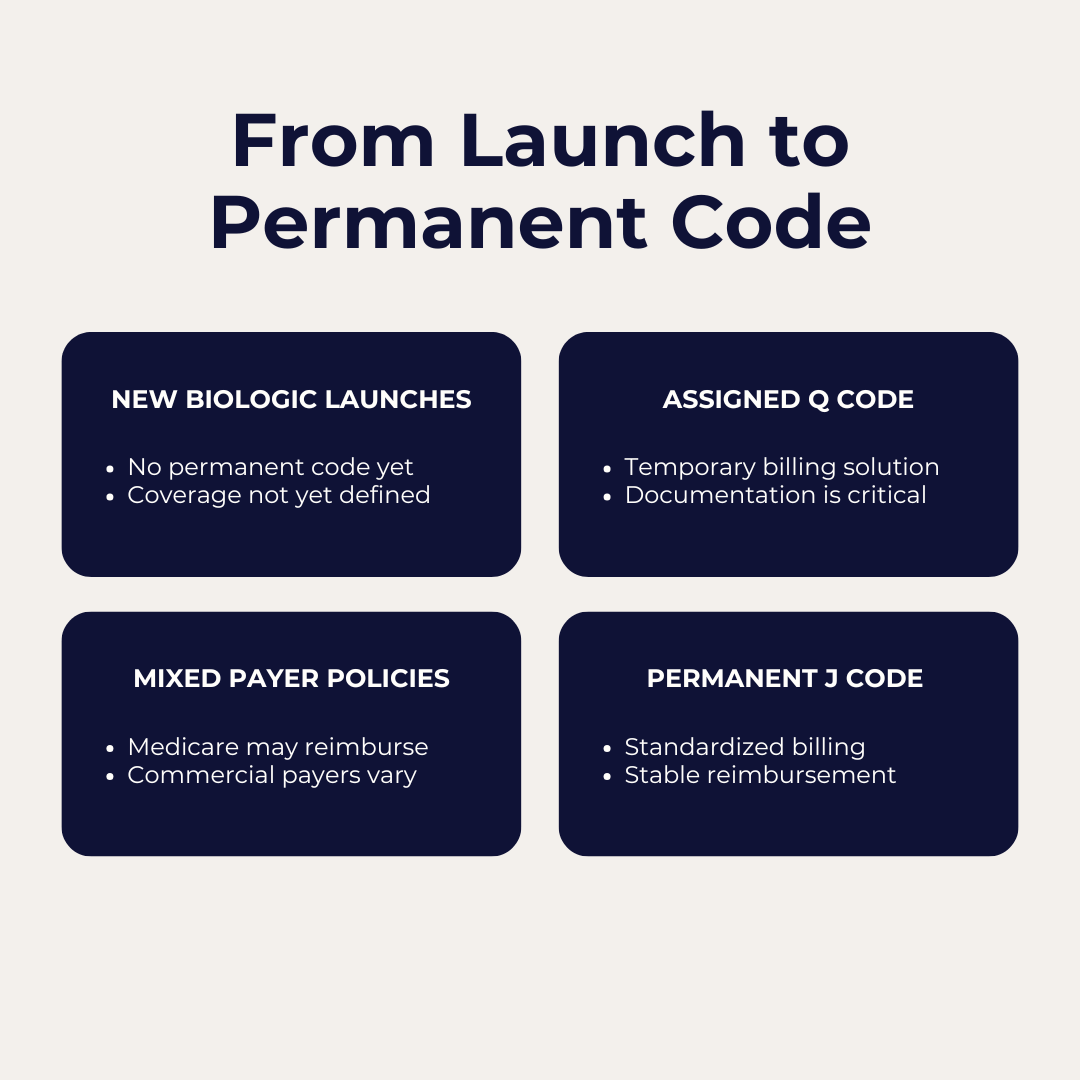
Q codes are also HCPCS Level II codes, but they are temporary. CMS uses them to designate new or emerging products that do not yet have a permanent J code. They often apply to biologics, injectables, or amniotic skin substitutes used in wound care and dermatologic surgery.
Think of Q codes as a bridge. A new product may begin its reimbursement life with a Q code, and over time, if CMS grants permanent status, it transitions to a J code. Until then, the only way to get paid for using that product is by billing the correct Q code. If your practice misses it, or if your team assumes there is no code yet, you risk absorbing the cost of a high-dollar product with no reimbursement in return.
Practices also need to be cautious when it comes to coverage. Not every Q code is automatically reimbursed. Checking the Local Coverage Determination (LCD) for Skin and Soft Tissue Substitutes is essential before purchasing these products. As of May 2025, there is a long list of Q codes still considered experimental and not covered by certain payers, including commercial carriers such as UnitedHealthcare. Failing to verify coverage in advance can result in significant financial loss even if the claim is coded correctly.
Practices should not assume that all Q codes are reimbursable. Many skin and soft tissue substitutes remain listed as investigational or non-covered under Local Coverage Determinations. Before purchasing these products, always confirm the most recent LCD guidance and payer policy to avoid costly denials.
Common Dermatology Q Codes
| Code | Description | Dermatology Use Case |
| Q4100 | Skin substitute, not otherwise specified | Catch-all for unlisted amniotic or synthetic skin substitutes used in wound care or dermatologic surgery. |
| Q4101 | Apligraf, per sq cm | Bioengineered skin substitute for chronic wounds, venous ulcers, and diabetic foot ulcers, sometimes managed by dermatologists. |
| Q4102 | Oasis wound matrix, per sq cm | Collagen-based skin substitute used in dermatologic wound care. |
| Q4106 | Dermagraft, per sq cm | Human fibroblast-derived skin substitute for chronic wounds. |
| Q4110 | PriMatrix, per sq cm | Fetal bovine dermal tissue for wound management and grafting. |
| Q4111 | GraftJacket, per sq cm | Acellular dermal matrix sometimes used in reconstructive dermatology. |
| Q4116 | AlloSkin, per sq cm | Human allograft skin substitute. |
| Q4121 | Theraskin, per sq cm | Cryopreserved human skin allograft for wounds. |
| Q4122 | DermACELL, per sq cm | Acellular dermal matrix used in dermatologic grafting. |
| Q4132 | Grafix Core or GrafixPL, per sq cm | Cryopreserved placental membrane grafts used in dermatology wound healing. |
| Q4133 | GrafixPRIME, per sq cm | Similar application as above, different formulation. |
| Q4137 | AmnioBand, per sq cm | Amniotic membrane graft used in wound care and surgical dermatology. |
| Q4149 | Excellagen, 0.1 cc | Flowable wound matrix for chronic wound care. |
| Q4150–Q4199 series | Multiple amniotic/placental skin substitutes | Wide range of amniotic products relevant to dermatology and wound healing. |
| Q4200+ series | Newer amniotic and regenerative tissue products | Frequently updated; critical for practices using advanced wound care therapies. |
Tracking the Lifecycle of J and Q Codes
J and Q codes move through stages as products evolve, from initial assignment to permanent status. Monitoring each phase protects reimbursement accuracy and helps prevent denials.

CPT Skin Substitute Grafts
In addition to assigning the correct Q code for the product itself, practices must also report the corresponding CPT code for the skin substitute procedure performed. These codes define the service provided and must be paired correctly with payer requirements to secure full reimbursement. Below is a listing of the CPT codes most commonly used in dermatology.
Code | Description |
15271 | Application of skin substitute graft to trunk, arms, or legs, total wound surface area up to 100 square centimeters; first 25 square centimeters or less. |
+15272 | Each additional 25 square centimeters of wound surface area, or part thereof (add-on code with 15271). |
15273 | Application of skin substitute graft to trunk, arms, or legs, total wound surface area greater than or equal to 100 square centimeters; first 100 square centimeters, or 1 percent of body area of infants and children. |
+15274 | Each additional 100 square centimeters of wound surface area, or part thereof, or each additional 1 percent of body area of infants and children (add-on code with 15273). |
15275 | Application of skin substitute graft to face, scalp, eyelids, mouth, neck, ears, orbits, genitalia, hands, feet, or multiple digits, total wound surface area up to 100 square centimeters; first 25 square centimeters or less. |
+15276 | Each additional 25 square centimeters of wound surface area, or part thereof (add-on code with 15275). |
15277 | Application of skin substitute graft to face, scalp, eyelids, mouth, neck, ears, orbits, genitalia, hands, feet, or multiple digits, total wound surface area greater than or equal to 100 square centimeters; first 100 square centimeters, or 1 percent of body area of infants and children. |
+15278 | Each additional 100 square centimeters of wound surface area, or part thereof, or each additional 1 percent of body area of infants and children (add-on code with 15277). |
Why These Codes Matter in Dermatology
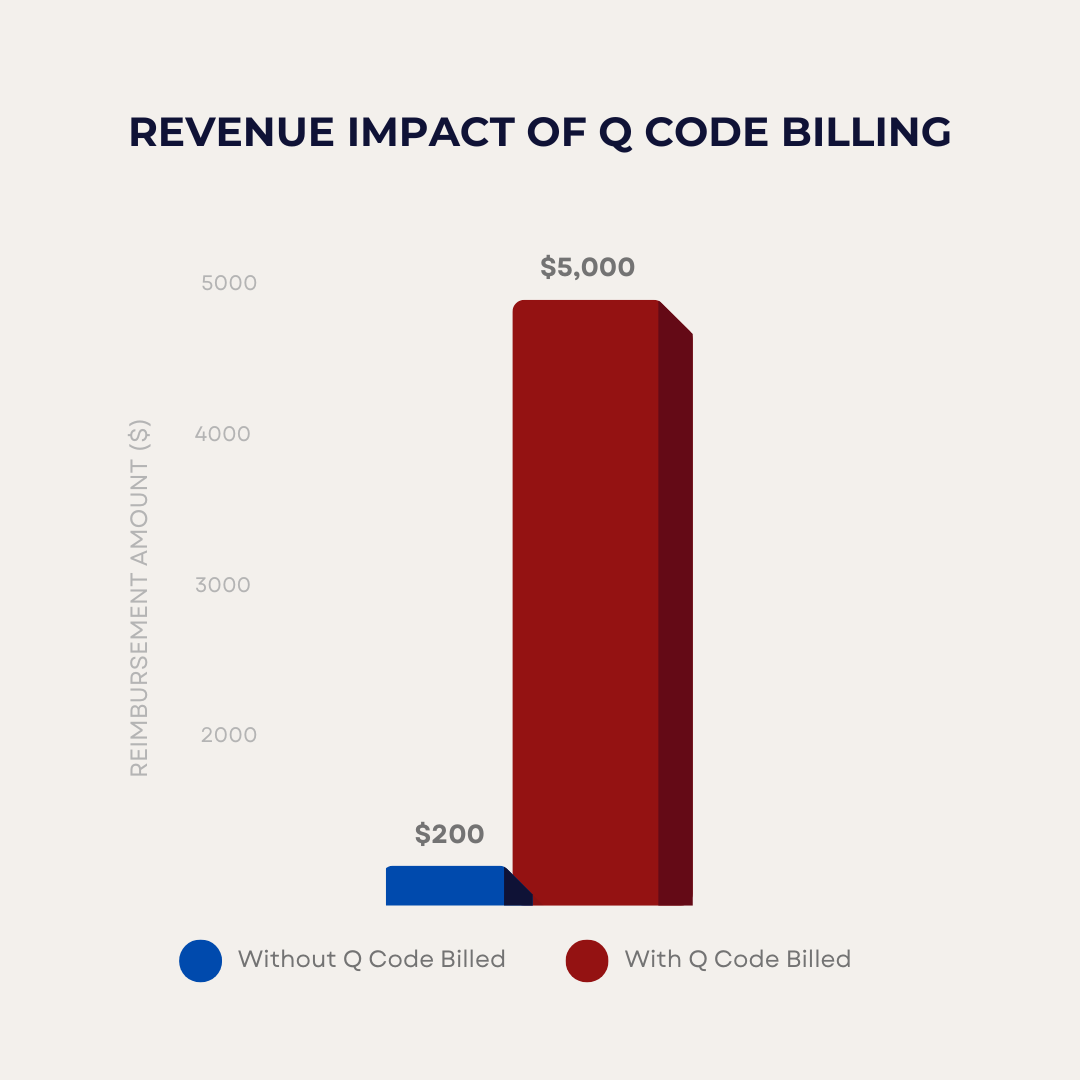
Both J and Q codes represent high-cost line items. Unlike a routine office visit or a simple procedure, the financial stakes are higher. When you purchase a biologic or an amniotic graft, you are taking on the expense up front. If you bill incorrectly, the cost sits on your books with no reimbursement.
From a billing company’s perspective, these codes are often separated in contracts with dermatology practices. Many agreements line out J and Q codes and apply a smaller percentage fee, recognizing that they involve different financial dynamics than office visits or procedures. Without this clarity, practices may feel that the billing company is profiting disproportionately on pass-through costs, while billing companies risk confusion when these high-dollar claims hit the system.
The lesson is straightforward. If you miss the code, you miss the money.
The Financial Impact: Real-World Scenarios
Consider two dermatologists, Dr. Anderson and Dr. Jones.
Example 1
Dr. Anderson administers an amniotic skin substitute that requires a Q code. Her billing team enters the correct CPT procedure code for the application but fails to include the Q code for the product. Although both procedures are properly documented and the CPT code is reimbursed, the claim for the high-cost skin substitute is denied. The result is a significant and avoidable revenue loss for the practice.
Example 2
Dr. Jones ensures that both the procedure and the Q code for the tissue are documented and submitted together. Her claim is reimbursed in full, covering both the service and the high-dollar supply. The complete and accurate claim submission, supported by thorough documentation, not only secures appropriate payment but also reduces audit risk. Even if the practice were audited, the documentation should prevent negative outcomes.
Staying Current with J and Q Code Updates
One of the biggest challenges practices face is that Q codes are constantly evolving. A product that has a Q code today may transition to a J code tomorrow. Staff who are not aware of the change risk billing the wrong code, resulting in denials and delays.
Payers also vary in how they handle Q codes. Medicare may reimburse promptly, while commercial carriers may have additional requirements or refuse coverage altogether until permanent status is granted. That variability makes it critical for practices to:
- Check payer policies regularly.
- Monitor CMS updates for coding changes.
- Educate staff on the importance of capturing lot numbers, units, and product details in the medical record.
Best Practices for Dermatology Practices
To make sure your practice is getting paid appropriately, consider the following approaches:
- First, verify codes before billing. Do not assume a new product has no code. Check CMS and payer updates.
- Second, carve out J and Q codes in contracts. This avoids disputes and ensures transparency by applying appropriate percentages or flat fees that reflect the unique financial impact of these codes.
- Third, audit claims regularly. Review a sample of J and Q code claims to confirm that both the service and the product are being billed correctly.
- Finally, educate the entire team. Clinical staff should understand why these codes matter. Documentation at the point of care is often the difference between successful billing and costly denial.
Looking Ahead: The Future of J and Q Codes in Dermatology
As biologics and regenerative therapies continue to expand in dermatology, J and Q codes will only become more common. Payers are scrutinizing these claims more closely than ever, given their high cost. Practices that fail to adapt risk not only financial loss but also compliance issues if they submit claims incorrectly.
The practices that thrive will be those that build internal systems for staying current, treat J and Q code billing with the same care as procedures and E/M visits, and work with billing partners who understand how to protect revenue streams tied to these products.
J and Q codes may not be the most talked about part of dermatology, but they are among the most important for your practice’s financial health. These codes capture high-cost drugs, biologics, and tissue products that, when billed correctly, can mean the difference between reimbursement and a substantial loss.
The question every practice should be asking is whether these codes are being billed accurately and consistently. Even a single oversight can leave thousands of dollars uncollected.
This is where having the right support makes a difference. At Inga Ellzey Billing Companies, our team is trained to stay on top of evolving J and Q code requirements, payer policies, and contract carve-outs. We help practices protect today’s revenue while preparing for tomorrow’s changes in reimbursement.