If your dermatology practice has been feeling the financial squeeze, you’re not alone. At both the 2025 American College of Mohs Surgery (ACMS) and the AAD Innovation Academy meetings, we heard the same concern echoed repeatedly: reimbursement cuts, especially from Medicare, are straining practices nationwide.
Physicians expressed frustration, uncertainty, and in some cases, resignation. The overarching theme? “We’re doing more for less.” And they’re right. CMS fee schedule reductions over the past several years have been steadily eroding margins, leaving practices scrambling to adapt.
At Inga Ellzey Billing Companies, we’ve seen how small reductions in reimbursement rates, while seemingly minor on the surface, can add up over time and result in significant decreases in provider revenue while the workload stays the same. In this article, we’ll break down what’s happening with CMS, how it’s affecting dermatology practices in 2025, and what your practice can do to protect its bottom line.
CMS Cuts: The Numbers You Can’t Ignore
Over the last five years, Medicare’s Physician Fee Schedule (PFS) has faced ongoing downward adjustments. The conversion factor, which is the dollar amount CMS pays per relative value unit (RVU), has declined overall since 2020. These small changes add up over time and can significantly affect provider revenue.
| Year | Conversion Factor |
| 2020 | $36.09 |
| 2021 | $34.89 |
| 2022 | $34.61 |
| 2023 | $33.89 |
| 2024 (Jan–Mar) | $32.74 |
| 2024 (Mar–Dec) | $33.29 |
| 2025 (final) | $32.35 |
These cuts impact more than just Medicare. Many commercial payers use the CMS fee schedule as a baseline when setting their own rates. If you haven’t already, this is the time to look at how your top procedures are being reimbursed.
In fact, understanding these changes isn’t just important, it’s essential. Practices that don’t routinely monitor fee schedules may not realize the extent of their revenue loss until it’s too late to reverse course. Budget forecasting, provider compensation planning, and even hiring decisions can be affected by small but persistent reductions. Now is the time to take a proactive stance.
2026 on the Horizon: What Dermatology Practices Should Know
CMS has proposed a modest recovery in the 2026 Physician Fee Schedule, with the conversion factor projected to rise to $33.42 for most physicians and $33.59 for those qualifying under Advanced Payment Models (CMS Fact Sheet). On the surface, that looks like a 3 to 4 percent increase compared to 2025.
For dermatology, the impact is less straightforward. CMS has also proposed a new 2.5 percent efficiency adjustment on work RVUs for non–time based services (CMS Fact Sheet). This includes many dermatology procedures. In addition, CMS wants to reduce practice expense RVUs for facility-based services to reflect the trend of dermatologists practicing in larger systems rather than private offices. Both of these changes could reduce the benefit of the higher conversion factor.
CMS is also proposing significant changes to how skin substitutes are classified and reimbursed. Under the 2026 rule, they would be treated as “incident-to supplies,” which could reduce reimbursement by as much as 90 percent for these products (Maynard Nexsen Summary). This is a major concern for dermatologists who use amniotic or other advanced wound products in their practices.
In short, 2026 may not deliver the relief that the higher conversion factor suggests. Dermatology practices should expect continued pressure on revenue and plan accordingly.
Top 20 Dermatology CPT Codes: Reimbursement Trends
Here is a comparison chart showing historical and projected reimbursement for common dermatology codes. These rates are approximations and should be verified using your practice’s payer-specific fee schedules.
Note: The rates shown here are based on Medicare data and are subject to Geographic Practice Cost Indices (GPCI) adjustments. Actual reimbursement may vary depending on your location and payer contracts. Always verify rates using your specific fee schedules.
CPT Code | Description | 2020 Rate | 2024 Rate | 2025 Rate |
11102 | Tangential biopsy of skin | $100 | $97 | $92 |
11103 | Additional tangential biopsy | $53 | $49 | $46 |
11104 | Punch biopsy | $125 | $121 | $116 |
11300 | Shaving epidermal/dermal lesion (0.5 cm or less) | $99 | $97 | $92 |
11301 | Shaving epidermal/dermal lesion (0.6-1.0 cm) | $121 | $118 | $113 |
12002 | Simple repair, scalp/trunk (2.6-7.5 cm) | $114 | $114 | $110 |
12011 | Simple repair, face/scalp (2.5 cm or less) | $113 | $112 | $108 |
12031 | Intermediate repair, scalp/trunk (2.5 cm or less) | $253 | $256 | $246 |
12032 | Intermediate repair (2.6 – 7.5 cm) | $303 | $296 | $286 |
17000 | Destruction of premalignant lesion | $65 | $66 | $64 |
17003 | Destruction benign lesions (up to 14) | $6 | $6 | $6 |
17004 | Destruction of 15+ premalignant lesions | $158 | $163 | $157 |
17110 | Destruction benign lesions (up to 14) | $111 | $110 | $106 |
17262 | Mohs micrographic surgery, first stage | $177 | $175 | $169 |
17311 | Mohs, first stage, head/neck/hands | $665 | $664 | $644 |
17313 | Mohs, 3rd stage | $622 | $623 | $605 |
88305 | Pathology interpretation | $69 | $69 | $67 |
96573 | Photodynamic therapy | $207 | $214 | $201 |
99213 | E/M Office Visit (established, low) | $75 | $90 | $88 |
| 99214 | E/M Office Visit (established, mod) | $109 | $127 | $124 |
Disclaimer: The rates shown here are based on the 2025 Medicare Physician Fee Schedule for Florida. Past rates are estimated for comparison purposes and may vary by locality or payer. Practices should verify rates using their own contracted fee schedules.
5 Revenue Strategies That Work in 2025
These cuts are here, and practices need to adapt. The good news? There are concrete steps you can take to protect your bottom line. Here are five that we recommend based on what we see across hundreds of dermatology practices.
1. Review Your Fee Schedules and Contracts
Make it a priority to review your top 20 CPT codes across Medicare and your top commercial payers. We often find that practices are unaware of significant disparities in what they’re getting paid for high-volume procedures.
Knowing your numbers gives you leverage when it comes to renegotiating payer contracts. Don’t rely on outdated schedules. Take the time to run the reports or have your billing company do it.
Consider running side-by-side comparisons of payer reimbursements across your top procedures. In many cases, it’s not just about the rate, it’s about whether you’re being paid correctly and consistently. And if you’re not, you may have the leverage to request a contract review.
2. Strengthen Your Modifier Usage
Modifiers are critical for accurate dermatology billing and can have a direct impact on reimbursement. We often see practices miss out on revenue simply by not applying modifiers correctly or not applying them at all.
Focus on reviewing common dermatology modifiers like 25, 59, and 76 to ensure they’re being used appropriately. Proper modifier use can prevent unnecessary denials and make sure you’re getting paid fully for the services you provide.
Need a refresher? Check out our Dermatology Billing Modifiers Guides
3. Optimize Patient Collections
When payer reimbursement shrinks, patient collections matter more than ever. Make sure you’re:
- Verifying eligibility before the visit
- Setting payment expectations upfront
- Offering text-to-pay and online options
Simple tools like front-desk scripting and real-time eligibility checks can drastically improve your cash flow.
Don’t underestimate the power of training your front office team. If staff are uncomfortable discussing costs or unsure how to handle objections, your practice will miss out on revenue that’s already due. Equip your team with scripts, offer financial estimate forms, and review balances prior to patient arrival.
4. Audit Your Coding Annually
Coding accuracy is one of the most overlooked areas where revenue is lost. Practices often under code or misuse modifiers, and that adds up.
We routinely identify missing charges or patterns of under coding that result in thousands of dollars left on the table. A coding audit doesn’t just protect your compliance, it can boost your revenue, too.
For example, one multi-location dermatology practice we work with identified $85,000 in missed opportunities in just one quarter after a routine E/M audit. With a few documentation changes and modifier training, that revenue was fully recoverable moving forward.
5. Streamline Your Billing Workflow with Smart Tools
It’s time to rethink your billing tools. Whether you’re billing in-house or outsourcing, incorporating smart automation makes a difference. Look for billing software or services that include:
- Denial pattern tracking
- Real-time claim validation
- Reporting dashboards with actionable insights
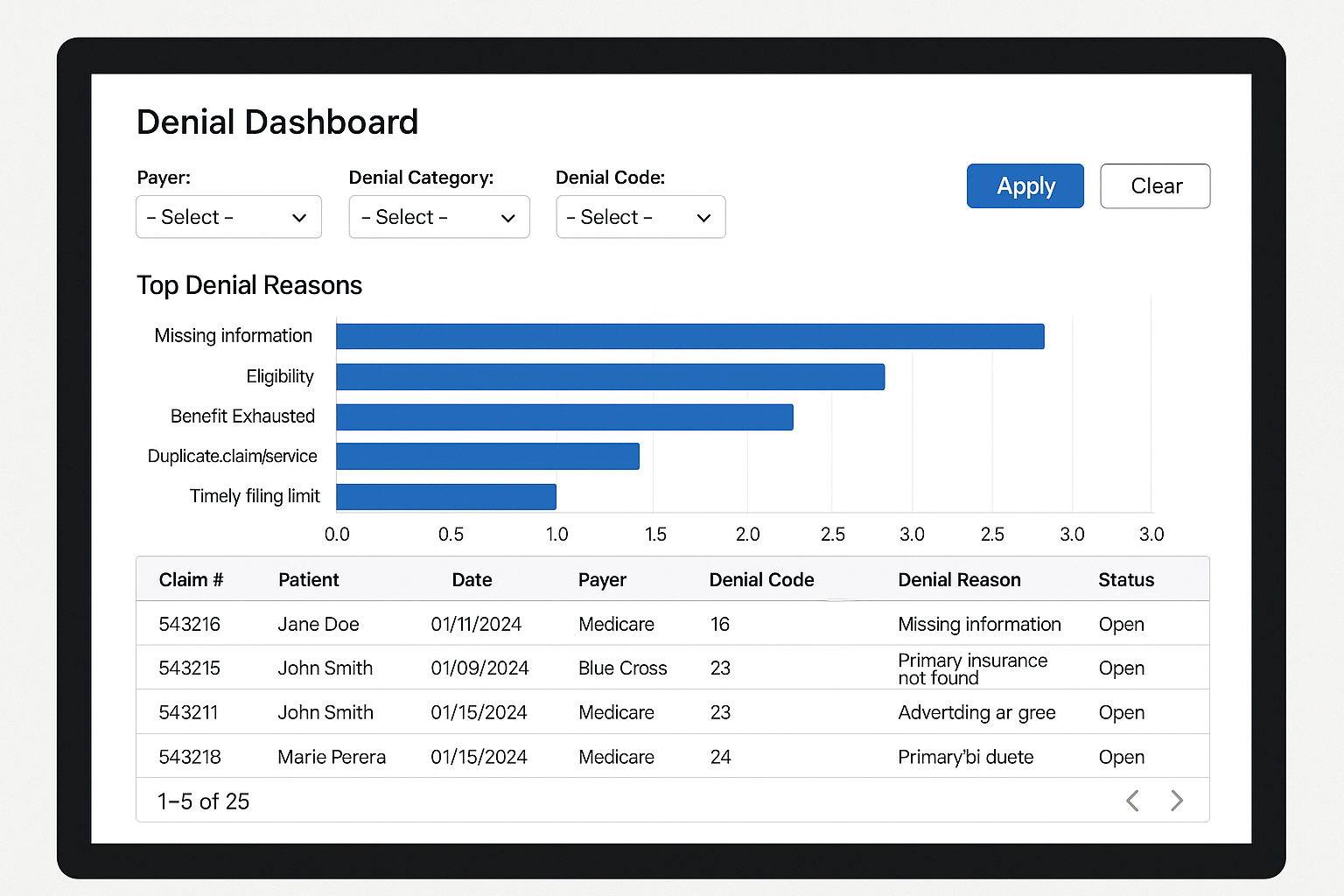
At Inga Ellzey Billing Companies, our internal processes help monitor underpayments and identify denial trends so our clients don’t have to chase every dollar manually. It’s part of how we help dermatology practices stay ahead of reimbursement trends.
CMS fee schedule cuts are not a temporary problem. They are part of an ongoing shift in healthcare reimbursement. Practices that don’t adapt will feel the impact.
The good news is that with the right strategy, you don’t need to take these cuts lying down. Review your coding. Rethink your contracts. Use the right tools. And above all, partner with a billing team that is looking out for you.
Need help understanding where your practice stands? Contact us for a complimentary revenue review of your top 10 CPT codes.
Read more from our published resources:
G2211 in Dermatology Billing: How to Maximize Reimbursement and Avoid Denials
2025 Dermatology Billing & Coding Updates
ABOUT INGA ELLZEY AND OUR DERMATOLOGY BILLING SERVICES
After 28 years of perfecting billing processes, Inga Ellzey continues to be the nation’s leading expert in dermatology billing. Our billing service serves over 100 dermatology practices in 37 states without utilizing any offshore labor. Our goal is to provide our clients and their patients with the most competent and professional service available on the market today.
If you are interested in speaking with our company about how we can maximize your collections while also improving your process, please contact us or call 888-434-4374.