Many dermatologists in private practice have a Mohs surgeon(s) as part of their group. Practices that have a large Medicare population and/or support other dermatology practices in the area that do not have a Mohs component, can significantly increase their practice revenues by offering this method of lesion removal.
Coding for these services is relatively simple once you understand the nuances of Mohs, repairs, biopsies, and histology. Correct coding ensures that the services are not bundled which could result in denials or trigger costly carrier audits.
Check our website for complete material regarding the various facts and guidelines associated with Mohs. You and your billing staff are advised to read through and understand the guidelines and information.
Caveats: In the following examples, the size of the lesions, defects, or repairs will be assumed as correct per the CPT codes used in the examples. Coordinate the description of the surgeries performed with the completed CMS-1500 form. Pay strict attention to modifiers and units! The use of modifiers -59, -76, and -XS can be used differently with different carriers. Billing staff should monitor denials, which indicate which modifier should be used, or go on the carrier’s website for information regarding modifier preferences. The examples used in these examples reflect the most common use of the modifiers. In all my examples, I show the use of modifiers -59 or –XS. Keep in mind that modifier -76 may be the modifier preferred by a carrier(s) in your area. Check carefully for carrier guidelines.
Modifiers -59 and -XS are used to represent two procedures performed in the same encounter but on different organs or structures. For example, a provider performs a destruction of an Actinic Keratosis on the patient’s cheek as well as a biopsy of the left arm. Modifier XS would be applied to the biopsy code.
The code, which receives the -XS modifier, is based on the bundling as indicated by the Correct Coding Initiative. Check your contracted carrier preference to see whether -59 or -XS should be used.
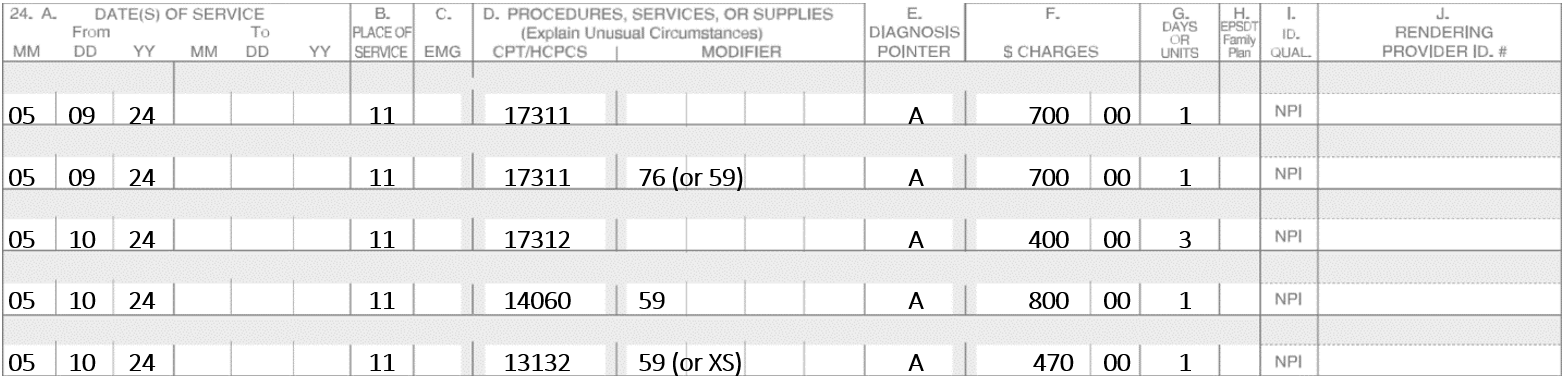
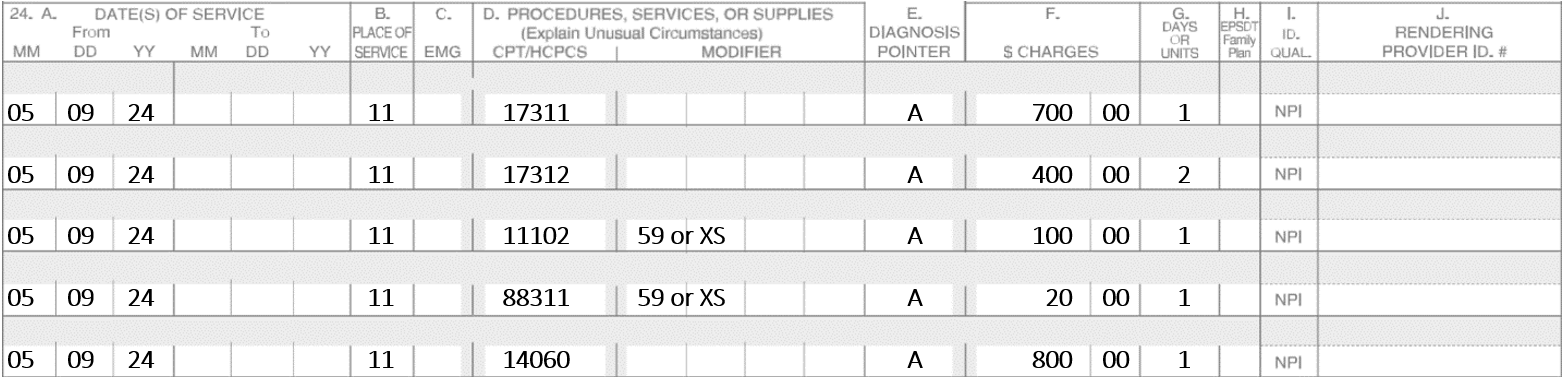
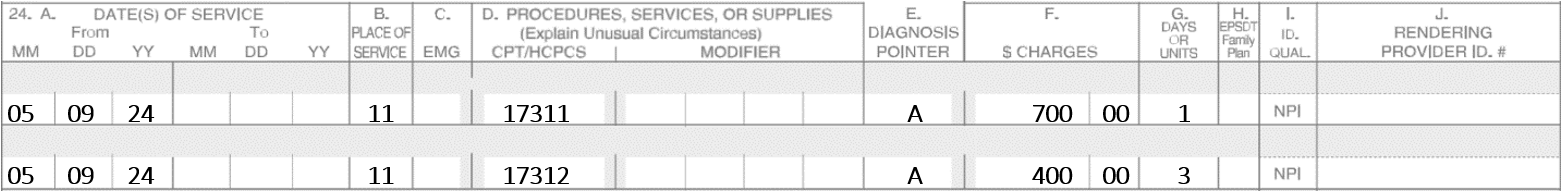
Example #1
A patient was seen with two lesions. Lesion one was on the right cheek and lesion two was on the left forehead. Lesion one had three stages of Mohs and was repaired with an adjacent tissue transfer. Lesion two required two stages of Mohs and was repaired with a complex linear repair.
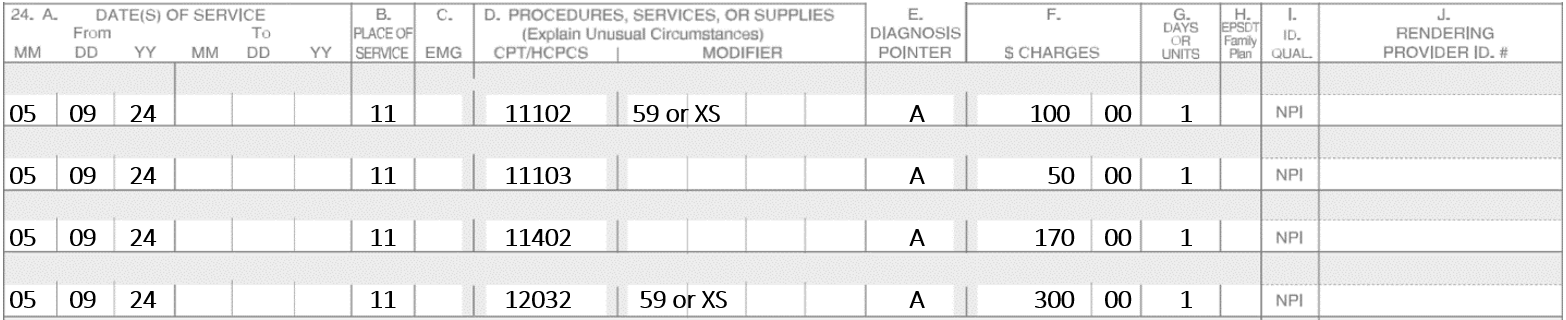
Example #2
A patient was seen for a lesion on the left side of the nose. The lesion was repaired with a full-thickness graft. Five stages of Mohs were required to obtain clear margins. The patient got extremely tired so it was decided to continue the following day.
On day two, two more stages were performed and then the defect was repaired with a full-thickness graft. The donor site was the back of the neck.
Example #3
A patient was seen for a lesion on the nasolabial fold. The patient was referred by their regular dermatologist for Mohs. There was no pathology report to confirm the diagnosis, so a confirmation biopsy was performed using a frozen section. The lesion was positive for Basal Cell Carcinoma. Two stages of Mohs were performed before clear margins were obtained. The resulting defect was repaired with an adjacent tissue transfer.
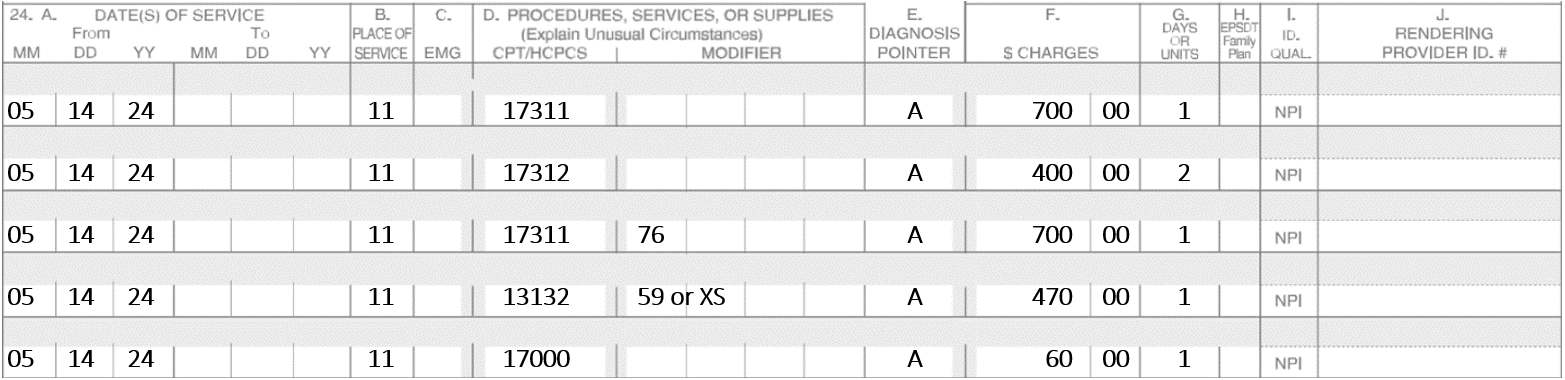
Example #4
A patient was seen for an annual check-up. During the examination, the physician saw two suspicious lesions that were biopsied to rule out Basal Cell Carcinoma. The biopsied lesions were on the forehead and the left side of the neck. A third lesion of the left arm was a compound nevus that was excised and closed with an intermediate repair.
The biopsy reports were received five days later. One was Actinic Keratosis and the other lesion was indeed a Basal Cell Carcinoma. The patient was scheduled for Mohs the following day.
On 5-14-2024, two stages of Mohs were performed on the lesion of the forehead that was repaired with a complex linear repair. On the lesion of the neck, one stage was performed. The lesion was also repaired with a complex liner repair. The Actinic Keratosis was destroyed using Liquid Nitrogen.
Note: When multiple open wounds are repaired, add together the lengths of those in the same classification and from all anatomic sites that are grouped in the same code descriptor. For example, if a wound is repaired from the neck and another from the hand, the length of both repairs are added together. If you bill each separately, one of the closures will be denied. The groupings are listed in the CPT codebook.
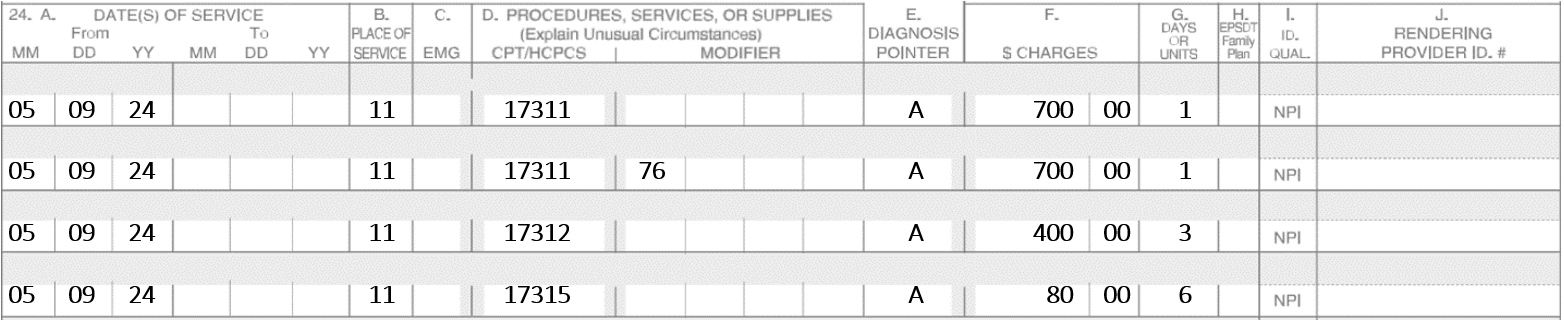
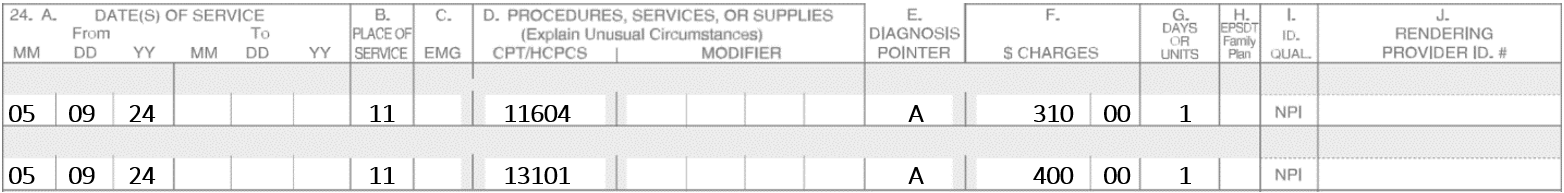
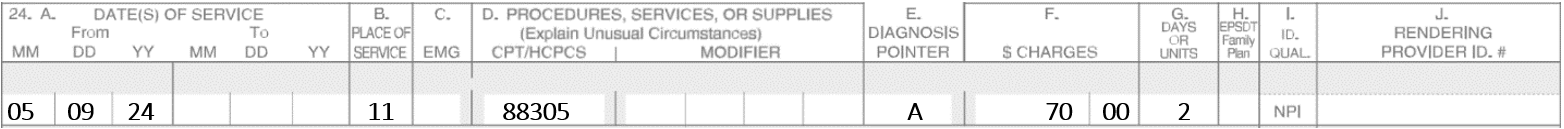
Example #5
Additional Tissue Blocks: Code 17315 replaces 17310 for additional tissue blocks. They are no longer referred to as specimens; they are now called tissue blocks. Use one unit for each additional block after the first five.
On 5-9-24, the patient presents two Basal Cell Carcinomas. One is on the nose and the other lesion is on the left upper lip. The nose requires three stages. In stage one there were six tissue blocks, in stage two there were six blocks and in stage three had only three blocks. The left upper lip requires two stages. Stage one had nine blocks and stage two had six blocks. Assume the repairs are not performed on the same date.
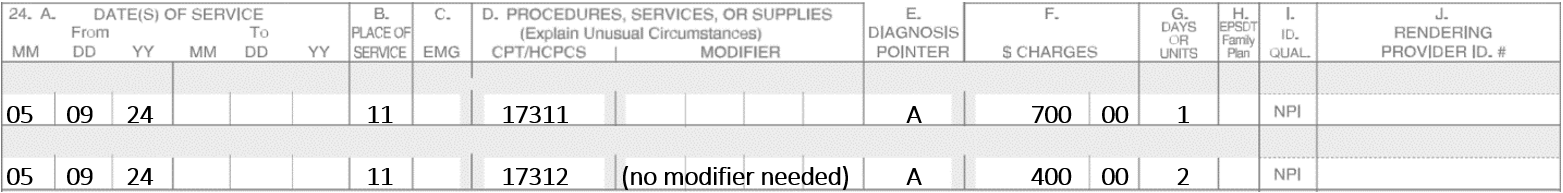
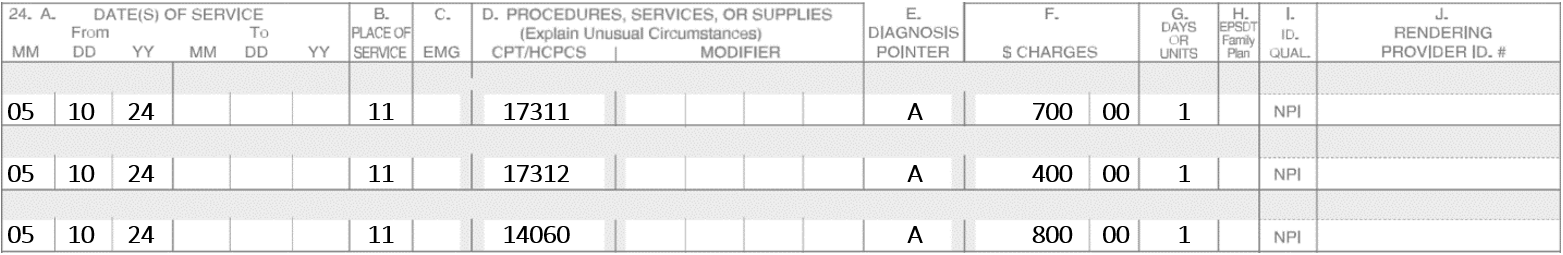
Example #6
A Mohs surgeon does Mohs on 5-9-24 on a Basal Cell Carcinoma of the upper lip. Four stages are performed, and margins continue to show incomplete margins. The patient is exhausted and cannot continue. The patient is scheduled for 5-10-24 to complete the Mohs. On 5-10-24, the patient returns, and two more stages are performed which show complete removal of the lesions. An adjacent tissue transfer is utilized to repair the defect.
Note: On 5-10-24, you must bill 17311 again. The post-op modifier -79 is not needed since the Mohs codes have -0- postoperative days.
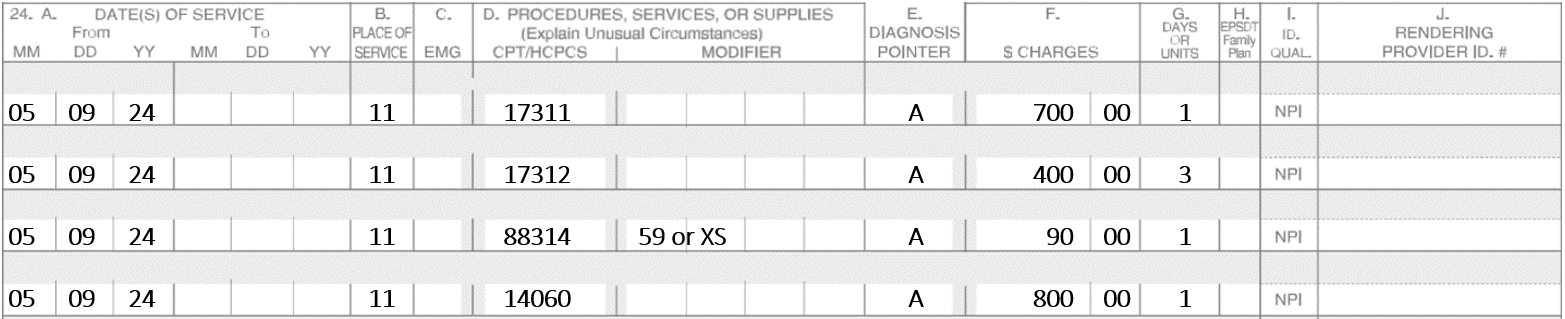
Example #7
A patient has four stages of Mohs performed on a lesion of the left ala nasi. A special stain was performed. To repair the defect, an adjacent tissue transfer and complex repair (e.g., CPT code 13151) were required.
Note: The complex linear repair cannot be billed since it is bundled with 14060 per the Correct Coding Initiative.
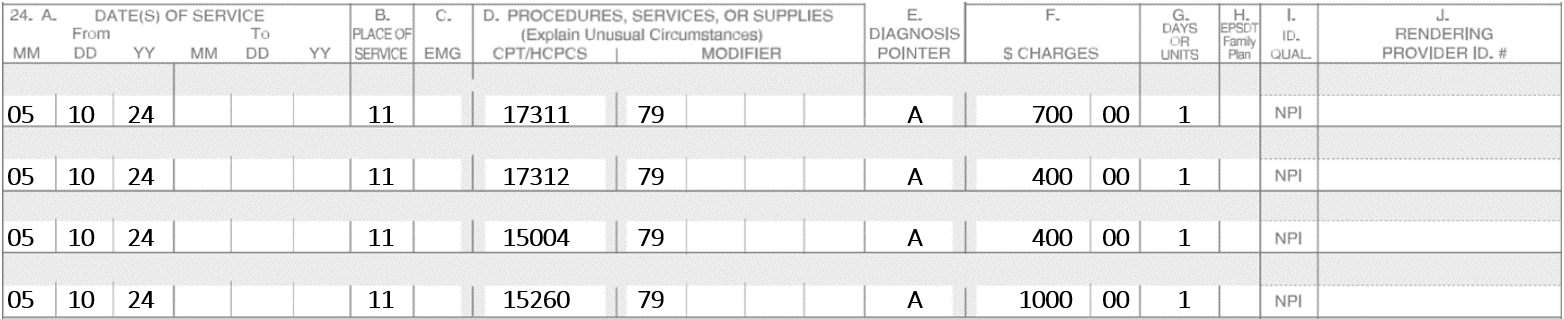
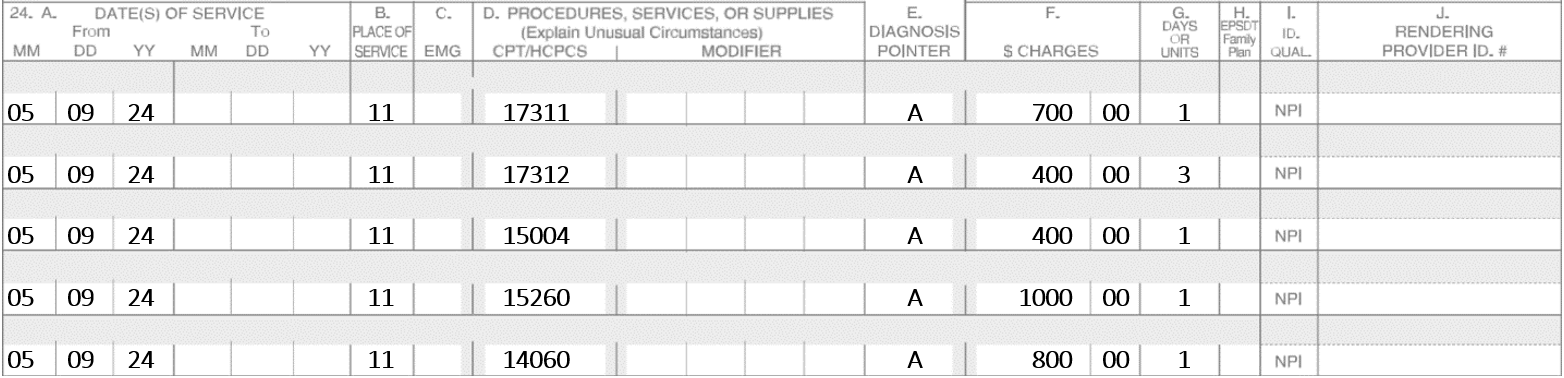
Example #8
A patient has four stages of Mohs performed on a lesion of the left ala nasi. To repair the defect, a full-thickness graft and an adjacent tissue transfer were required.
No modifiers are needed as the repairs are both performed on the same lesion.
Documentation – Important
On October 27, 2020, Medicare clarified if the tumor is visualized on stage one, you must describe the histology of the specimens taken. That description should include:
- Depth of invasion
- Pathological pattern
- Cell morphology
- Perineural invasion
- Presence of scar tissue.
Note: Here’s a sample of the Mohs Flow Sheet that includes the necessary documentation components.
Special Stains
- If additional special pathology procedures, stains, or immunostains are required, use 88311 – 88314, and/or 88342.
- Do not report 88314 in conjunction with 17311 to 17315 for routine frozen sections stain (e.g., hematoxylin and eosin, toluidine blue) performed during Mohs surgery.
- When a non-routine histochemical stain on frozen tissue is utilized, report 88314 with modifier 59. This is the most common coding for this scenario.
Permanent Stains – Pay Attention to This!
- Do not report 88302 to 88309 on the same specimen as part of the Mohs surgery.
- No charges can be billed for permanent sections done in conjunction with Mohs that are reported by an outside entity.
- If a Mohs surgeon sends a final “stage” or specimen of tissue to an outside lab or even to the practice’s in-house lab, and the entity bills for any pathology:
- The Mohs surgeon must pay for the permanent section
- No entity can submit payment
- If another provider seeks payment for the permanent section, the Mohs codes will be denied
“Slow Mohs”
Sometimes a Mohs surgeon performs a procedure that they consider a “Slow Mohs.” There is no such thing. One of the key “ingredients” of Mohs is regarding histology by use of frozen sections, which must be performed by the Mohs surgeon, not another provider. A technician can be utilized to prepare the slides, but not read them.
Dr. Smith, a highly qualified Dermatologist, explains the process very clearly. For example, if immunostains are performed on a Lentigo Maligna and the dermatopathologist in the practice reads the slides and is able to process the immunostains and reports the results in just a couple of hours, the Mohs code cannot be billed?
Per the definition of Mohs per the CPT book, Mohs requires that the surgeon also serve as the pathologist. If another pathologist reads the slides, whether the dermatopathologist is a part of the group or not, it is not Mohs.
For billing purposes, this procedure is considered a staged excision with the pathology services reported separately by the pathologist. If all of the stages were accomplished on the same day, an excision would be reported as a single excision with the final diameter reported as the excised diameter.
If for example, the final excised diameter is repaired with an adjacent tissue transfer, the excision of the malignant lesion is included in the adjacent tissue transfer code and cannot be reported separately. Therefore, the only code that would be reported by the surgeon on this date of service would be the adjacent tissue transfer. Per the AMA/CPT 2023, the adjacent tissue transfer code descriptor states “The excision of a benign lesion (11400 – 11446) or a malignant lesion (11600 – 11646) is not separately reportable with codes 14000-14302.”
Although dermatologists know what “slow Mohs,” means, it is suggested that this term is not used in the medical record, as it will confuse auditors. Instead, refer to the procedure as excision with margin control.
If “slow Mohs” stages take more than one day to perform, the final excised diameter would be reported on the first day, and the additional margin diameter would be reported on the second day with a 58-modifier indicating that this procedure was staged. Keep in mind:
- True Mohs surgery has a zero-day global period, but “slow Mohs,” reported as the excision of a malignant lesion has a 10-day global period.
- An adjacent tissue transfer has a 90-day global period and includes excision of the malignant lesion if performed on the same date of service.
- If a complex closure is required, rather than an adjacent tissue transfer, the lesser valued code would be subject to multiple surgery reduction if the two procedures were performed on the same date of service.
Example #9:
A patient was scheduled for the removal of a Malignant Melanoma on the left arm that was confirmed by a biopsy taken two weeks prior. The surgeon removes a segment of skin that is 1.0 x 2.5 cm/d. The practice has a dermatopathologist in the group so he prepares the slides, not under the frozen section, and reports the margins are still dirty. Later, the same day, another piece of tissue is removed resulting in a final defect of 1.3 x 3.25 cm/d. The defect is repaired with a complex linear repair. The following CPT codes are billed.
Separate Claim Form for Dermatopathologists
Read more from our published resources:
MAXIMIZING PROFIT FOR MOHS SURGEONS
CODING AND DOCUMENTATION GUIDANCE FOR MOHS SURGERY REIMBURSEMENT
UNDERSTANDING THE ROLE OF MODIFIERS IN MEDICAL BILLING
ABOUT INGA ELLZEY AND OUR DERMATOLOGY BILLING SERVICES
After 28 years of perfecting billing processes, Inga Ellzey continues to be the nation’s leading expert in dermatology billing. Our billing service serves over 100 dermatology practices in 37 states without utilizing any offshore labor. Our goal is to provide our clients and their patients with the most competent and professional service available on the market today.
If you are interested in speaking with our company about how we can maximize your collections while also improving your process, please contact us or call 888-434-4374.